Demystifying information on pregnancy, fertility,
and all the things about our ladyparrts
About me
Contact me
Labia and Labiaplasty
As part of Female Health Education, Dr. Quimby and I led a health education class at a local girls’ private high school. We wanted the talk to be straight from gynecologists, different than others they had heard. As part of it, we showed real photos of external female genitalia (images previously printed in the medical literature). The point? Let them see what normal vulvas look like! No other person has seen more vulvas than a gynecologist and we are the best equipped to give reassurance that variations on anatomy are normal and expected.
What happens when something does not look anatomically normal though, or if it is a normal variation but causing symptoms and problems in that person’s body? It depends on what body part we’re talking about of course, and it depends on the issues that are arising. Sometimes the answer is corrective surgery. And when we talk about the vulva, and more specifically the labia, that corrective surgery is called a labiaplasty.
That’s my topic today and here’s what you’ll find:
- A quick anatomy lesson
- Medical reasons for labiaplasty
- Considerations for cosmetic labiaplasty
ANATOMY
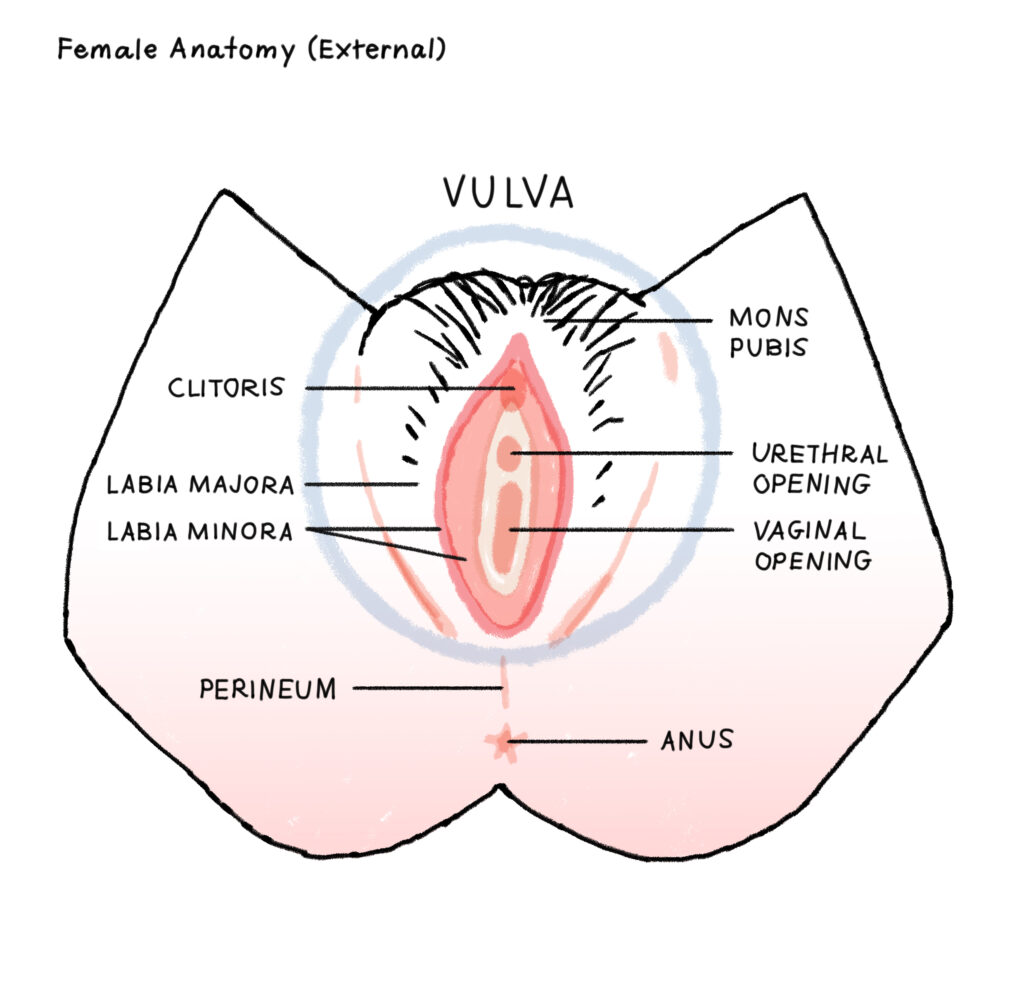
The vulva is the external part of female genitals. Here’s an illustration to help identify the various components and organs that make up the vulva.
- The mons pubis is the top, somewhat fatty part on top of the pubic bone (covered with pubic hair).
- There are 2 sets of “lips” of the vulva – the labia majora and labia minora.
- The labia majora is the set that grows pubic hair, the most visible.
- The labia minora is the set of lips inside the labia majora – these are smaller, more sensitive, delicate tissue and do not grow pubic hair.
The vulva also includes: Clitoral hood and clitoris (the most important organ of female genitalia for sex but not one we will be discussing today; urethral opening; vaginal opening called the introitus; vaginal vestibule – the entry into the vagina, just inside the introitus.
Other components like Bartholins glands and Skenes glands that are less obvious (this article about Bartholin glands cysts and abscess is my most read article).
~ A quick word about slang terms for the vulva ~
The overused “slang” of saying vagina instead of vulva is truly problematic. Example: “My vagina hurts after that wax.” You definitely mean the vulva. If your cosmetologist is waxing your vagina please run far far away.
I don’t have an issue with slang for genitals in and of itself– as long as it’s used with good humor and by adults for adults (kids should be learning the proper terms before starting to use nicknames or slang).
There are plenty of slang terms and nicknames for male genitalia : balls / nuts / cojones / sack / family jewels for testicles; cock / dick / rod / weenie / peter / prick / johnson / schlong for penis. I have no problem with these (besides some being gross) because each of these slang terms is for a specific and anatomically distinct body part. No one is using a slang “testicles” to describe a penis. No one says “penis” when they mean testicles. “Penis” and “testicles” are not used interchangeably as part of slang vernacular.
Why is it different with female anatomy? Why do we say “vagina” instead of vulva and so often refuse to say the term “vulva” altogether? Because of lack of knowledge? See above for anatomy lesson. Because our genitals are more complex? Pathetic excuse. Because the vulva is treated as an enigma or some “secret” that should not be spoken out loud? Those days are past. Let’s use accurate language. Let’s learn proper female anatomy. Let’s empower ourselves by not being embarrassed by the names of our organs. Let’s teach our kids (our daughters) their crucial and important body parts.
Take this as a plea from me – use the correct term. My daughter is growing up using the term vulva to describe her vulva. Unfortunately sometimes she also refers to my Volvo as a vulva too – but that’s a different post (but btw – she’s not embarrassed when she accidentally says that).
Moving on to the main topic: Labiaplasty
Labiaplasty is surgical repair of the labia. There are 2 sets of labia, as described above: labia majora and labia minora. Labiaplasty almost always refers to labia minora and the “surgical repair” is to reduce its size.
Why is labiaplasty done?
The primary medical diagnosis for labiaplasty is “labia minora hypertrophy” which means enlargement of the labia minora. The problem is the lack of a standardized definition of “enlargement”, so it turns into a judgment, an opinion that the labia are enlarged, not an actual fact. It often means that one or both of the labia minora extend past the labia majora, but there is no specific measurement, size, or criteria to say how far beyond the labia majora the labia minora needs to extend to consider it hypertrophied. In one study looking at anatomy in females, more than 50% of females had “labia minora hypertrophy”. This statistic alone tells us extension of the labia minora past the majora is not an abnormal enlargement but a common, expected, normal anatomic variation of the vulva. I can tell you from the gazillion pelvic exams I’ve done in my career, there is vast variation in appearance and size of the labia majora and minora.
The follow up question is then: If it’s normal, why would there be a medical indication for surgical repair?
When labia minora “hypertrophy” exists, extending past the protective labia majora, there’s the possibility of irritation, pain, even infection of that delicate tissue. The pain and irritation are typically with exercise, when the friction of the labia against underwear and clothing is excessive.
A few of my patients have had these concerns too:
- Complaining that their labia minora is long enough to sneak outside or get caught on their underwear. You can see how this would be really uncomfortable and distracting.
- Interfering with sex is another one –the longer labia minora gets pulled or tethered.
- I once had a patient with a very thin skin tag hanging from her labia minora, about 1 centimeter long. It had grown over the course of a few months, likely an inflammatory response to injury of the tissue. It was getting caught when she wiped after peeing, during sex, and sometimes just putting on underwear, causing pain and even more inflammation and irritation. I removed it with a quick office procedure. The pathology? Labia minora hypertrophy.
Considerations for Cosmetic Requests for Labiaplasty
Cosmetic procedures is a layered topic in general. The goal with procedures solely on the focus of cosmetics – what something looks like – is to make the individual person undergoing the procedure feel better about their appearance. Sometimes fixing the one feature that is causing someone distress – be it their nose, boobs, labia, or whatever – really, truly fixes the problem. Sometimes, however, that feature was a temporary focus of that person’s dissatisfaction with themselves and when it’s cosmetically altered, the fixation turns to some other body part. Over and over again. The root of the problem is their view of their body as whole, not just that one specific body part. They need to work on their brain to improve their body image. In this population, cosmetic surgery is working on the wrong body part.
In a culture with a heavy emphasis on appearance AND where porn is widely available, the appearance of a hairless, small vulva and labia is often thought of as the ideal appearance, especially for heterosexual men. Females are then pressured, either overtly or discretely, to obtain this “ideal”. This is where cosmetic requests for labiaplasty come in.
Cosmetic labiaplasty is then fraught with this question – will the surgery actually be helpful? What if it still doesn’t look like their ideal? For these complicated reasons, many cosmetic surgeons require patients to have a psychologic evaluation and be older than 18 years old prior to a cosmetic labiaplasty.
Don’t get me wrong – I think there is a role for cosmetic labiaplasty. I also think cosmetic labiaplastys are sometimes done for a bad reason. Any cosmetic procedure may turn out to be the most important surgery of someone’s life and help restore their confidence … or it can be a useless surgery with the potential for complication and lifelong regret. That’s a lot to consider.
Having a Labiaplasty – details about the procedure itself
The surgeon will explain the procedure, reviewing potential risks and expectations for recovery. This is typical of any surgical procedure. While the point of surgery is to fix whatever problem is occurring with the labia, there is no guarantee that the patient will be 100% happy with the results. While that’s the ultimate hope, improvement in symptoms is the goal.
The labiaplasty procedure itself is done in a procedure or operating room with anesthesia. The part of the labia minora that extends beyond the labia majora is removed with a scalpel and then sutures placed. Anatomy is assessed throughout. After care usually involves modified activity for up to 2 weeks: avoiding irritation to the area by wearing loose clothing and avoiding certain exercises or activity that can put friction on the sutures. Topical anesthesia like lidocaine spray or gel is often recommended too. As the sutures dissolve it is common to have itching or burning and is important to not rub or scratch the healing area as well.
And that’s the end of your lesson!
I’d be happy for you to share your experience if you feel comfortable!
ADD A COMMENT
Aug 21, 2024
Original post published:
* Content reviewed annually for accuracy
Leave a Reply
Submit Form
Want to chat more? Email me directly or fill out the form below!
I cannot respond to patient inquiries (insurance, scheduling, requests for appointments) or requests for medical advice.
You can contact my office at (310) 423-1224 for more information.
If you are an existing patient, message me through your patient portal.
I’m delighted to share how I successfully overcame the Herpes virus using natural medication {HERBS}. Through a native local medicine prepared by Doctor Awase, I managed to suppress the virus and improve my overall well-being at the first week. Two weeks into taking the medication, I became fine totally and no more single outbreak/symptoms. Today, I’m living a fulfilling and Herpes-free life.![cured] Confirmed by my Doctor after going for a medical checkup. I am herpes free. Demonstrating that natural approaches can offer effective solutions for health challenges such as herpes. He also cures HPV, PCOS, Fibroid, Endometriosis and lots more. See how to reach out below.
WhatsApp +2349074997110
Email:- dr.awaseherbalhome@gmail. com
HOW I WAS CURED FROM HERPES VIRUS
I am writing this testimonial with immense gratitude and a renewed sense of hope in my heart. For years, I battled with the physical and emotional torment caused by the herpes virus. It felt like an unending struggle, until I discovered a remarkable solution that changed my life forever. Like many others, I had tried countless remedies, medications in search of a cure. I had lost hope, resigned to the belief that herpes was something I would have to live with indefinitely. However, fate intervened and led me to a breakthrough that altered the course of my life. Upon stumbling on a revolutionary treatment option, my skepticism slowly transformed into a flicker of hope. The treatment was a natural remedy from Dr Awase [ HERBS ] Over time, as I followed the treatment diligently, I started noticing positive changes and I experienced a boost in my overall well-being. I am ecstatic to share that I am now herpes-free confirmed by my Dr after a test was done. The treatment I received was nothing short of miraculous and I couldn’t be more grateful. I have regained my self-confidence and the burden that once weighed heavily upon me has been lifted. I was cured of my herpes virus through natural medication.
If you, like me, have been struggling with herpes and searching for a way out, please know that hope exists. May my story inspire hope in the hearts of those who need it. He also specializes in getting rid of HPV, OVARIAN CYST, PCOS, HEPATITIS and a lot more.
Contact on WhatsApp +2349074997110
Email:- dr.awaseherbalhome@gmail. com
This article is truly insightful and well-written—I appreciate the valuable information shared here!
I wanted to share my own experience, hoping it might help others in a similar situation.
My husband and I invested $250 in a promising opportunity we found online. Our initial investment quickly grew by 30%, prompting us to increase our stake to $97,700 over time. However, when we tried to withdraw our profits, we were surprised by a 40% upfront commission demand. Unable to meet this unexpected requirement, I sought advice from friends who recommended professional help. I contacted them on Telegram, sharing all the investment details. Fortunately, they intervened effectively, recovering our initial investment and profits. Their support was crucial during a challenging period.
For anyone facing a similar situation, seeking expert assistance is vital.
Email: (marciagarci52@(gmail. com
I already gave up on ever getting cured of HSV2 because i have try many treatment none of them work out for me i have gone to different hospital they always tell me the same thing there is no cure for herpes, when i came across a post about Dr UMA in the net from a lady called Angela i contacted her and she reassured me with his herbal medicine which i took according to the way he instructed, that how i was cured. I doubted at first because i have been to a whole lot of reputable doctors, tried a lot of medicines but none was able to cure me. so i decided to listen to him and he commenced treatment, and under two weeks i was totally free from Herpes. i want to say a very big thank you to DR UMA for what he has done in my life. feel free to leave him a message on email dr.umaherbalcenter@gmail.com or also Whats-app him +2347035619585.. he also cure all this 1.HIV 2.HIV HPV 3 .ALS 4. BED WETTING DIABETES.
Do you find your problem hard for you? Infertile or Heartbroken? Are you finding it difficult looking for a reliable herbal healer to cure your sickness? I say this because I have been helped by Lord Krish Spiritual in restoring happiness into my life. My Mom had been sick with Stage 4 Melanoma Cancer which nearly took her life. I was sad because of this sickness and I didn’t know what to do to save my mother’s life. I would never have met Lord Krish if my friend had not introduced him to me by telling me about a herbalist who has helped so many people worldwide and it’s true. I contacted Lord Krish at lordkrishshrine@gmail.com and within 3 days, I received herbal medicine from him through a courier and I used it on my mom. Within a week, mom was cured and healed. I would advise anyone out there to Contact Lord Krish at lordkrishshrine@ gmail. com and meet him to help you with any sickness you are passing through