Demystifying information on pregnancy, fertility,
and all the things about our ladyparrts
About me
Contact me
Vulvo-what-ia???
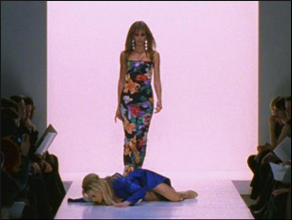
Sex and the City repeats are on and this episode was yesterday. Don’t lie to me – you probably recognize this phrase! It’s only one of the best episodes (Carrie falls on her face during the fashion show).
Charlotte sees her obgyn for “burning, stinging, itching” and is diagnosed with vulvodynia. She is prescribed an antidepressant and goes on her way. When she’s explaining her diagnosis later – that her “vagina is depressed” – the ladies have no idea what she is talking about.
So what is vulvodynia? Is it a real diagnosis, or just made-for-TV?
It’s a real medical diagnosis, and can be serious and debilitating in its worst form. But it’s not a straight forward or well defined problem either, and the diagnosis and treatment differ from one doctor to another. Basically, it’s pain in the vulvar region that can’t be explained by inflammatory, infectious, cancerous, or neurologic causes. That means it is a diagnosis of exclusion: all these reasons need to be ruled out before vulvodynia is ruled in.
That’s one problem in reaching the diagnosis: many tests and studies need to be done before you get the diagnosis. Patients get frustrated when the tests come back normal. The symptoms are bothersome and they know something is wrong – they want to know why the tests aren’t proving anything.
Another problem: patients often have difficulty describing their symptoms in detail. Symptoms are usually vague and generalized. Women may say it’s burning, itching, stinging, raw, constant. The severity of these symptoms differ from woman to woman.
Many of the symptoms are similar to a yeast infection, which happens to be the most common cause of vulvar pain. Women treat themselves without relief, and sometimes worsen the symptoms by doing so (topical yeast infection treatment, especially the shorter courses, can definitely cause irritation).
Am I alone?
If you have these symptoms, you are not alone. We think about 15% of women will have varying degrees of vulvodynia sometime during their lives. The National Vulvodynia Association puts this number at one in four women!
What causes it?
We don’t exactly know. We think it is related to estrogen in some way (women often experience vulvar pain when they are going through menopause). It may be from pelvic floor muscle dysfunction (the same muscles you use when doing your Kegal exercises). It may also be from a long standing neurologic injury, like an injured pelvic nerve during childbirth. The pain persists even when the injury is better (which is why no neurologic cause can be identified at time of evaluation).
So what is the treatment?
It varies, and there are many options.
- Vulvar care sounds simple (sometimes too simple) but it should not be underestimated: Avoid the use of scented products, like soaps or creams. Avoid tight, non-breathable clothing. Avoid activities and exercises like biking and horseback riding.
- If there are any ongoing sexual or psychological issues, counseling can help and needs to be initiated.
- Creams and ointments, like estrogens, steroids, or anesthetics, may be prescribed.
- Believe it or not, there are physical therapists who specialize in pelvic floor muscles. This kind of treatment may help, especially if the pain is getting in the way of sexual activity.
- And lastly, we get to Charlotte’s treatment: antidepressants. Certain types of antidepressants may help, and are usually used in conjunction with creams and ointments.
Of course we never hear about Charlotte’s vulvodynia after this one episode, which is not normal. Most women diagnosed with vulvodynia in real life should continue treatment and care long term, the way you would with any chronic pain problem. Real lifers: establish a relationship with your gynecologist, and follow up. As you can see, there is no one correct treatment, so you and your doctor can try different treatments until you find the best one for you.
Source: ACOG Committee Opinion
Up to Date. Clinical manifestations and diagnosis of generalized vulvodynia and Treatment of vulvodynia
Google the National Vulvodynia Association for patient information.
ADD A COMMENT
May 18, 2013
Original post published:
* Content reviewed annually for accuracy
Leave a Reply
Submit Form
Want to chat more? Email me directly or fill out the form below!
I cannot respond to patient inquiries (insurance, scheduling, requests for appointments) or requests for medical advice.
You can contact my office at (310) 423-1224 for more information.
If you are an existing patient, message me through your patient portal.
Do you find your problem hard for you? Infertile or Heartbroken? Are you finding it difficult looking for a reliable herbal healer to cure your sickness? I say this because I have been helped by Lord Krish Spiritual in restoring happiness into my life. My Mom had been sick with Stage 4 Melanoma Cancer which nearly took her life. I was sad because of this sickness and I didn’t know what to do to save my mother’s life. I would never have met Lord Krish if my friend had not introduced him to me by telling me about a herbalist who has helped so many people worldwide and it’s true. I contacted Lord Krish at lordkrishshrine@gmail.com and within 3 days, I received herbal medicine from him through a courier and I used it on my mom. Within a week, mom was cured and healed. I would advise anyone out there to Contact Lord Krish at lordkrishshrine@ gmail. com and meet him to help you with any sickness you are passing through